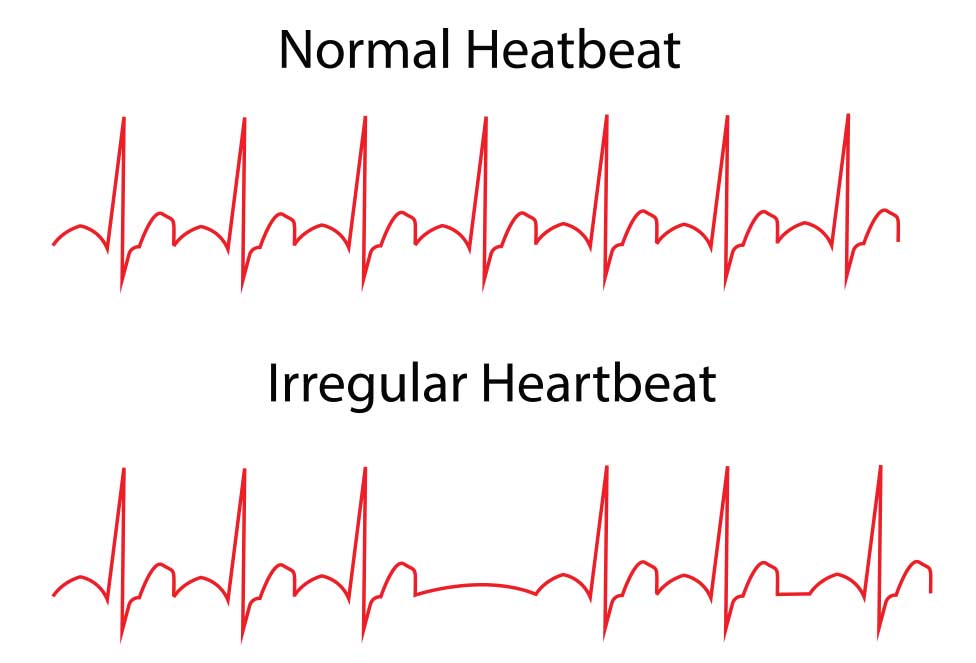
Most arrhythmias (abnormal heartbeats) neither cause symptoms nor interfere with the heart’s ability to pump blood. Thus, they usually pose little or no risk. They can cause considerable anxiety if a person becomes aware of them. There are some arrhythmias, harmless in themselves that can lead to more serious arrhythmias.
Any arrhythmia that impairs the heart’s ability to pump blood adequately is serious. How serious, depends in part on where the arrhythmia originates. Is it in the heart’s normal pacemaker, in the atria, or in the ventricles? Generally, arrhythmias which originate in the ventricles are more serious than those that originate in the atria. These are more serious than those that originate in the pacemaker. However, there are many exceptions.
For people who have a harmless, yet worrisome arrhythmia, reassurance that the arrhythmia is harmless may be treatment enough. Sometimes arrhythmias occur less often or even stop, when doctors change a person’s drugs or adjust the dosages. Avoiding alcohol, caffeine, smoking, or strenuous exercise can also help.
Antiarrhythmic drugs are useful for suppressing fast arrhythmias that cause intolerable symptoms or pose a risk. No single drug cures all arrhythmias in people. Sometimes several drugs must be tried until the response is satisfactory. Sometimes antiarrhythmic drugs can worsen or even cause arrhythmias; this effect is called proarrhythmia. Antiarrhythmic drugs can also produce other side effects.
Artificial pacemakers are electronic devices that act in place of the heart’s own pacemaker. These devices are implanted surgically under the skin, usually below the left or right collarbone. They are connected to the heart by wires running inside a vein. New circuitry has almost completely eliminated the risk of interference from automobile distributors, radar, microwaves, and airport security detectors.
Any abnormality within the chest is wise to get checked out by your family doctor.